What we can learn from medicine about fixing things without taking them apart.
A longtime friend who was suffering from extreme fatigue and shortness of breath. She was diagnosed with congestive heart failure caused by aortic valve stenosis, and she required an aortic valve replacement. This was a very big deal that required open-heart surgery. It involved cracking her chest, placing her on a heart-lung machine, stopping her heart, cutting into her aorta, surgically removing the defective valve, suturing a replacement valve (harvested from a pig) in its place, suturing her aorta, restarting her heart, and closing up her chest. Afterward, she spent a week in the hospital and more than two months recovering at home.
That occurred about 15 years ago. Now, the replacement valve is starting to give out, and she needs another valve replacement. This time, remarkably, the valve will be replaced without opening her chest or stopping her heart.
Nowadays, most aortic valve replacements are done using a technique called transcatheter aortic valve replacement or TAVR. A small incision will be made in her groin, and a guide wire will be passed up through the femoral artery into the aorta, and through the aortic valve using X-ray guidance. The guide wire will be used to guide a balloon-tipped catheter into the valve. The balloon will be inflated to open the worn-out valve completely. Then, a replacement valve pre-sewn into a metal stent will be passed through the catheter and positioned inside the old valve. The balloon will be inflated once again to expand the stent into place with the new valve inside it. Once the proper functioning of the new valve has been verified, the catheter will be withdrawn, and the small groin incision will be sutured. She’ll probably go home the next day and return to normal in a week.
The old open-heart approach was highly invasive. The new TAVR technique is a great example of minimally invasive surgery (MIS) that is far less risky and far less traumatic. There’s really no comparison.
My Own MIS Experience
Recently, I experienced this MIS revolution firsthand. It all started when I found myself briefly sidelined by a nasty case of diarrhea. It self-resolved after two miserable days, but I realized that this was my third encounter with gastrointestinal distress in the past year.
Being the data-driven fellow that I am, I asked my primary care physician if she thought some follow-up testing might be prudent. Being the data-driven doc that she is, she wrote me a prescription for some blood labs and another for an abdominal ultrasound. The blood labs showed a mildly elevated liver enzyme (ALT), and the abdominal ultrasound revealed a moderately dilated common bile duct (CBD), suggesting that something might be obstructing it—possibly a gallstone or a tumor. An abdominal MRI was ordered.
The MRI revealed a 17x12x8 millimeter gallstone in the CBD, which was dilated to 12mm in diameter (about twice normal). The medical tongue twister for this condition is choledocholithiasis. The stuck stone was obstructing the normal flow of liver bile into my duodenum, messing up my digestion and making my liver unhappy.
In the past, treatment of this condition would involve surgery—open or laparoscopic CBD exploration. Fortunately for me, there is now a minimally invasive interventional endoscopic procedure for removing gallstones from the CBD. Its medical term is unpronounceable—endoscopic retrograde cholangiopancreatography—which is why it’s always referred to by the acronym ERCP. I was scheduled for an ERCP two days after the MRI diagnosis.
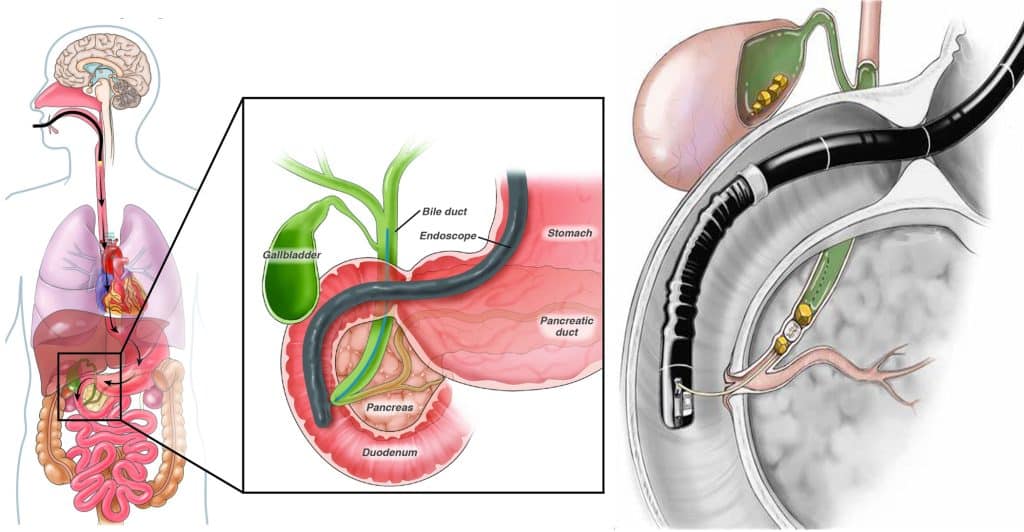
The ERCP is a complex and technically challenging procedure. It involves a side-viewing duodenoscope—basically a specialized borescope equipped with more tools than a Swiss army knife. The procedure is done with the patient under general anesthesia and is X-ray directed, so it requires a four-member team consisting of the gastroenterologist who specializes in endoscopy, an assistant (since it requires four hands), a radiology technician and an anesthesiologist.
An article from the National Institutes of Health that I found with Google stated that ERCP complications, such as acute pancreatitis, are significantly lower if the endoscopist has done the procedure at least 180 times before. Naturally, I checked on this and learned that my gastroenterologist had performed thousands of ERCPs, so I was satisfied I’d be in competent hands.
Once I was put to sleep with propofol, the scope was inserted through my mouth, esophagus, stomach, and pyloric valve into my duodenum (top of the small intestine). The ampulla—where the CBD discharges into the duodenum—was located visually through the scope. A guide wire was inserted through the ampulla and threaded into the CBD using X-ray guidance to ensure it was in the right place. A small incision was made to open the ampulla—referred to as a sphincterotomy. This permitted the stones to be extracted using various types of baskets or snares or—in my case—an inflatable balloon used to trawl the CBD and drag the stones through the ampulla into the duodenum. Two stones were found and extracted from my CBD. Then the scope was removed, the propofol was stopped, and I woke up 30 minutes later with a very mild sore throat. I was discharged about an hour later with instructions not to eat until the next morning.
By now you’re probably thinking, “What the heck does any of this have to do with aviation?”
MIS in Aircraft Maintenance
A&P mechanics are the surgeons of aviation. But unlike MDs, they have been slow to adopt minimally invasive procedures, particularly when it comes to piston aircraft engines. Cylinder removal is still the “standard of care” for most engine maladies. Many A&Ps are spring-loaded to call for an engine teardown whenever they change the oil and find metal in the oil filter.
Splitting the case of an aircraft engine is the aviation equivalent of open-heart surgery—it’s the most invasive thing you can do to an engine. Right behind it on the invasiveness scale is cylinder removal—a highly invasive and risky procedure that’s the aviation analog to the open gallbladder removal surgery (cholecystectomy) involving a six-inch abdominal incision. (This surgery very nearly killed my dad in the 1990s, which explains why I’ve been reluctant to have my own stone-filled gallbladder removed.)
For more than a decade, I’ve been on a campaign to sensitize A&Ps and aircraft owners to the risks of invasive maintenance and the importance of using minimally invasive procedures wherever possible to minimize that risk. I’ve evangelized using borescopes and other non-invasive methods to figure out what’s happening inside cylinders, crankcases, fuel tanks, and aerodynamic structures without taking them apart. I’ve also promoted minimally invasive therapy, such as lapping valves in place and performing solvent ring flushes to solve the most common cylinder issues without needing cylinder removal.
“For more than a decade, I’ve been on a campaign to sensitize A&Ps and aircraft owners to the risks of invasive maintenance and the importance of using minimally invasive procedures wherever possible in order to minimize that risk.”
At first, my sermons from the pulpit of the Church of Minimal Invasiveness were not well received by A&Ps. “Show me where this procedure is described in the maintenance manual,” they’d ask. “I’m not allowed to do something that isn’t approved by the manufacturer,” they’d say. I would patiently explain to them that the regulations—specifically 43.13(a)—do not limit them to following the manufacturer’s instructions. They explicitly permit them to use “other methods, techniques, and practices acceptable to the Administrator.”
In this context, the phrase “acceptable to the Administrator” means that the person using a particular method, technique, or practice must have a good-faith belief that the FAA would not find it unacceptable if and when they ever looked at it. Given that both the lap-valves-in-place and solvent-ring-flush procedures have been performed thousands of times without so much as a peep of objection from anyone in the FAA, it seems to me that any mechanic who wishes to use those procedures should be able to do so with a good-faith belief that they are acceptable to the Administrator.
Encouragingly, in the past few years, I’ve seen more and more A&Ps willing to try these minimally invasive methods. At first, they do them on a what-do-I-have-to-lose basis, skeptical that they’ll solve the problem but figuring that the cylinders can always be removed if they don’t. Then, after finding that these methods really do work, their skepticism evaporates, and they begin to embrace the procedures enthusiastically.
But most A&Ps still remain stubbornly skeptical, and many flat refuse to even try them. So, we’re not at the tipping point yet. But we’re making progress.
Complacency
Part of the problem is that most A&Ps do not, in my opinion, have an appropriate level of fear about the risks involved in cylinder removal and other invasive maintenance practices. They change cylinders every week and consider it a routine procedure. They become complacent—a word that Merriam-Webster defines as “self-satisfaction, especially when accompanied by unawareness of actual dangers.”
I wish more A&Ps could have shared my experience as an expert witness, consultant, or investigator on more than a dozen air crash cases in which an engine failed catastrophically shortly after undergoing the removal and replacement of one or more cylinders. I’m sure this experience would make them far less complacent.
Right now, as it happens, I’m involved as an expert witness on a case where a Cessna ditched in the ocean shortly after takeoff from a coastal Florida airport on the second flight after the #2 cylinder was changed. The professional pilot did a remarkable job of ditching, and the three occupants were rescued by a nearby pleasure boat after sustaining only minor injuries.

Just last week, I reviewed the final NTSB report involving the off-airport landing of a Cirrus SR22 whose engine threw the #4 and #5 connecting rods. The pilot deployed the CAPS parachute system once he determined the airplane wouldn’t make the destination airport in Lincoln, Nebraska, and landed in a hay field. The pilot and his passenger walked away uninjured (although the aircraft wasn’t as lucky).
The NTSB attributed the accident to the pilot’s decision to continue the flight to the planned destination rather than to land at a closer airport after the first indication of abnormal engine operation. However, the only plausible explanation for the simultaneous detachment of the #4 and #5 connecting rods is the displacement of the main bearing that supplies oil to the #4 and #5 rod bearings. The only plausible explanation for that is inadequate preload on the through bolts that clamp that main bearing in place. Maintenance records indicated that those two through bolts were torque-relieved and then re-torqued when the #5 cylinder was removed and replaced with a new cylinder 8 months and 250 hours before the accident. The NTSB didn’t attribute the engine failure to the cylinder change, but it’s hard for me to believe that the two weren’t causally connected.
Fortunately, these two accidents didn’t result in serious injury or death. Most of the other air crash cases I’ve been involved in where the engines cratered shortly after cylinder replacement, had far worse outcomes for the occupants. I’m absolutely convinced that the use of minimally invasive techniques would have prevented these accidents. Whether you’re an A&P or an aircraft owner, this should be serious food for thought.